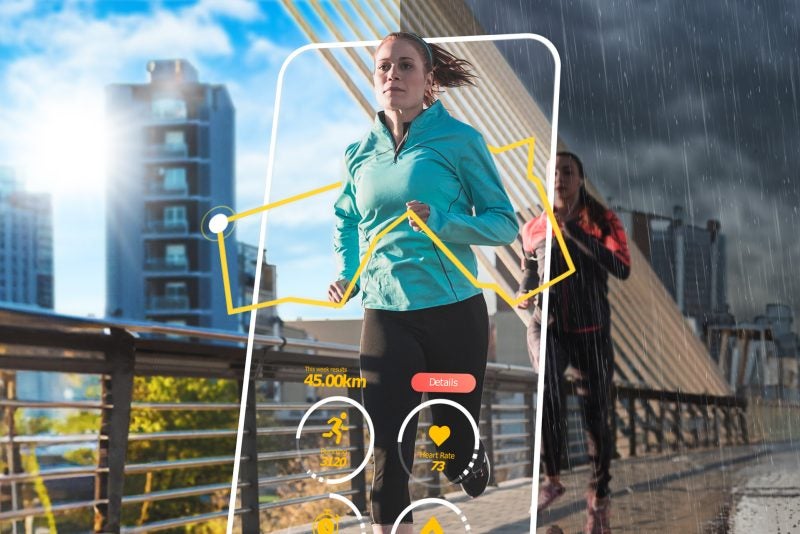
Every decade has an exercise trend or two that defines it. Step aerobics and the Thighmaster were popular in the ‘90s, for instance, while exer-gaming and CrossFit were all the craze in the 2000s. To know what’s trending this decade, look no further than your wrist (or to those around you) — chances are it’ll be adorned with some sort of wearable device, fitness tracker, or smartwatch.
“They started getting really popular six to seven years ago,” says Atreyi Kankanhalli, a professor at NUS Computing, who researches healthcare informatics. Kankanhalli purchased her first Fitbit in 2016 and has been wearing one ever since. “Now almost everyone I know is wearing some form of smartwatch or using some fitness app. It’s really caught on,” she says.
Wearables have altered our relationship with exercise — it’s made us more conscious of our step count, how many calories we’ve burnt, and how long we’ve spent sitting down. But how do they also impact the other pillar of healthy living — eating right?

“We know that mobile health apps can change eating behaviour and potentially lead to weight loss, better diabetes management and other health outcomes,” says Kankanhalli. “But what evidence is out there to support this? To what extent has the link between the two been studied? And where are the remaining knowledge gaps?”
Scouring databases
To answer those questions, Kankanhalli paired up with two others — Assistant Professor Hyelim Oh at Sogang University in Seoul and then-PhD student Jieun Shin, who now works at Samsung Research — to embark on a comprehensive literature search. They focused on studies of health apps that allowed users to log their food intake throughout the day.
The team scoured three health and medical databases, and found 30 journal papers that fit the bill. For each study, Kankanhalli and her team first analysed what kinds of data the app collected, and how this was done. Were users restricted to using only text to log their meals, or could they also snap pictures, take videos, and record voice notes? Apart from food intake, what other kinds of information did the app collect — did it ask for data on height and weight, users’ health goals, or prescribed medication?
The most common mode of input, the researchers found, was text. In other words, getting users to manually key in what they ate. Only a fifth of the studies examined used more advanced input modes, such as photo recognition and voice logging, they report in a journal article. That’s a shame, says Kankanhalli, because these other techniques can make tracking food intake much easier.
“When it comes to diet tracking, entering what you eat is very onerous. So, a photo-based method can make it more feasible,” she says. At the same time, she recognises how challenging it is to create algorithms that can figure out portion size, identify ingredients, and estimate calories.

“Say you take a photo of char kway teow,” says Kankanhalli, referring to the popular local dish of fried rice noodles, cockles, and prawns. “You can take a photo of it, but how do you estimate the portion size? How do you determine if someone added extra sauce? That is the challenging part.”
Additionally, the team also found that while all the apps in the reviewed studies collected data on diet intake, they didn’t always gather other types of information. However, such extra data (for example, body mass index and waist circumference) could benefit users by providing a better appreciation of how dietary changes alter their bodies and health.
Measuring the impact of interventions
Once they had looked at the apps’ data input, the researchers then turned to the interventions the studies offered. The most common intervention was providing users feedback on their progress (usually through the app itself, but sometimes through email, text, or other notifications).
In some instances, the feedback was tailored to the individual, which is valuable, says Kankanhalli. “Personalisation is understanding that different people will respond in different ways… so app developers can think about how they can provide such tailoring through the algorithms and features.”
In addition to giving feedback, the apps in some of the studies made diet tracking into a game of sorts, awarding points for various achievements or by setting quests and challenges to complete. In a few studies, the apps also allowed for users to review the goals they had set, while a handful provided educational material on food and dieting.
However, the apps in most studies were limited in terms of what they had to offer, says Kankanhalli. “Mobile apps of the future can definitely make better use of these various intervention categories.”
Lastly, the researchers looked at whether the 30 studies actually examined if the mobile health app in question led to changes in users’ dietary behaviour and health outcomes. One study, for example, found that mobile-based self-monitoring led to users eating more vegetables, which in turn resulted in weight loss. Another study analysed how having strong social support led to fewer calories consumed.

However, only five studies conducted such a causal impact analysis. And in most instances, impact was measured in terms of weight loss. But other health outcomes are important too, says Kankanhalli. For example, people with diabetes would want to know how changes in their eating habits affects their blood glucose levels.
Overall, studies either analysed healthy behaviour change (did the user eat more vegetables or consume less fat?) or directly measure health outcomes (did he or she lose weight?).
But a more useful analysis would systematically and statistically answer both these questions: How did the mobile app change food intake? How did these changes then improve various health outcomes?
“So, we want to understand if there are mediating effects, and how do these effects work?” says Kankanhalli. “Our aim was to uncover the gaps in previous studies, and point out the areas that require more investigation,” she says. As an example, she is currently working on personalising mobile health interventions based on temporal profiling of users.
At the end of the day, mobile health interventions are about “nudging people towards healthier behaviours, improving lifestyles, and outcomes for individuals and society as a whole – including reducing healthcare costs,” says Kankanhalli. “As Covid has shown, the baseline health of a person is very important in terms of whether they get a disease, and how well they recover”
“If we can do our little bit to nudge people in the right direction,” she says, “then it’s worth it.”
Paper:
Mobile-Based Interventions for Dietary Behavior Change and Health Outcomes: Scoping Review